Neglected Tropical Diseases (NTDs): Elephantiasis

More than one billion people in 149 countries are estimated to be affected by NTDs, which can lead to malnutrition, disability, and even death.
Neglected tropical diseases (NTDs) are a wide range of infectious diseases caused by bacteria, viruses, and parasites that affect people living in poverty worldwide, especially in tropical and subtropical areas like Asia, Africa, and South America.
Elephantiasis, often known as filariasis, is a neglected chronic disease caused by filarial worms that attack the lymph nodes and blood vessels.
People infected with this worm experience swelling in their legs and decreased lymphatic system function. As a result, their bodies have difficulty fighting germs and infections. The skin becomes hardened and thickened, resembling elephantiasis, which is why this disease is referred to as such.
In Indonesia, elephantiasis is caused by three filarial worm types: Brugia malayi, Brugia timori, and Wuchereria bancrofti. These worms can spread between humans through mosquito bites.
Worms that have infected the lymph nodes will spread to the blood vessels. When a mosquito bites someone with elephantiasis, the filarial worm parasite larvae are carried with the blood and enter the mosquito's body. For one to two weeks, the larvae transform the mosquito's body.
Then, the infected mosquito bites a healthy person. The larvae enter through the skin and go to the lymph nodes. There, the larvae grow into adults and live in the human body for 5-7 years. Adult worms mate, releasing millions of larvae called microfilariae into the blood.
People whose blood contains worms can spread the disease to others through mosquito bites.
Living in endemic areas, poor environments, and repeated mosquito bites raises the risk of developing the disease.
Symptoms
Some people do not show symptoms. However, some others may develop filarial fever, which manifests as lymphangitis (inflammation of the lymphatic system) and lymphadenitis (inflammation of the lymph nodes) with non-specific symptoms, such as headache, fever, chills, and malaise. Filariasis can cause lymphedema (fluid retention) or hydrocele (swelling of the scrotum).
The feet are the areas that are usually infected. Swelling and thickening of the body parts can cause pain and impaired mobility. Infected skin will also look dry, thick, ulcerated, darker, and mottled.
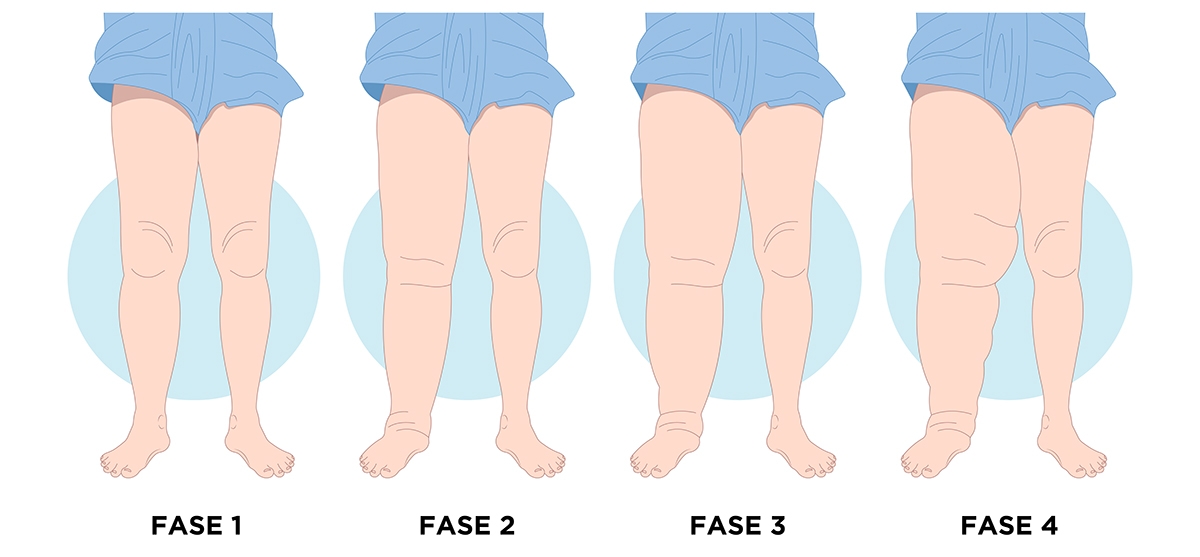
Elephantiasis symptoms can be categorized into different stages:
1. Asymptomatic phase
During this phase, the sufferer does not feel any symptoms. Often, people are unaware that they have been infected with filarial worms. The virus has harmed the lymphatic system and kidneys while weakening the immune system.
This asymptomatic phase causes patients to receive late treatment, and the condition develops into the acute phase.
2. Acute phase
The acute phase is defined by the appearance of local inflammation in the skin, lymph nodes, and lymphatic vessels as a response to the body's immune system to the parasitic infection that occurs. The sufferer experiences symptoms of fever, swollen lymph nodes, and legs, and even swelling of the scrotum in men.
3. Chronic phase
In the chronic phase, the lymph nodes begin to swell and thicken, especially the skin of the legs. Men have thickening of the scrotum, while women experience swelling of the breasts and vagina. Other symptoms of this disease include stiff and hard skin, pain in the swollen area, chills, fever, and feeling unwell.
Filariasis, if not treated, can lead to serious health problems. One is severe swelling in the infected area, resulting in pain.
Diagnosis
A blood test is the usual diagnostic method for elephantiasis. Because these worms are invisible to the human eye, medical workers will draw blood from the patient and examine it under a microscope. Sampling is usually done at night because these worms are active.
If needed, the doctor may conduct additional tests, including ultrasound or X-ray scans, and urine tests. A scrotal ultrasound can show the movement of adult worms in men who do not show symptoms.
The "filarial dance sign" is a worm movement pattern found in men's lymphatic vessels.
Treatment
To overcome swelling and discomfort, usually pain, elephantiasis can be treated and cared for by:
- taking antiparasitic drugs, such as diethylcarbamazine (DEC), ivermectin and albendazole
- cleaning the infected area with soap and water (antiseptic) to prevent infection
- raising the swollen body part
- treating wounds in an infected area
- exercise
- in some cases, surgery can be performed, such as reconstruction of the infected area or removal of lymphatic tissue.
Prevention
The best way to prevent elephantiasis is to avoid mosquito bites during the early morning and afternoon. Also, eliminate the mosquito breeding sites in and around your home.



